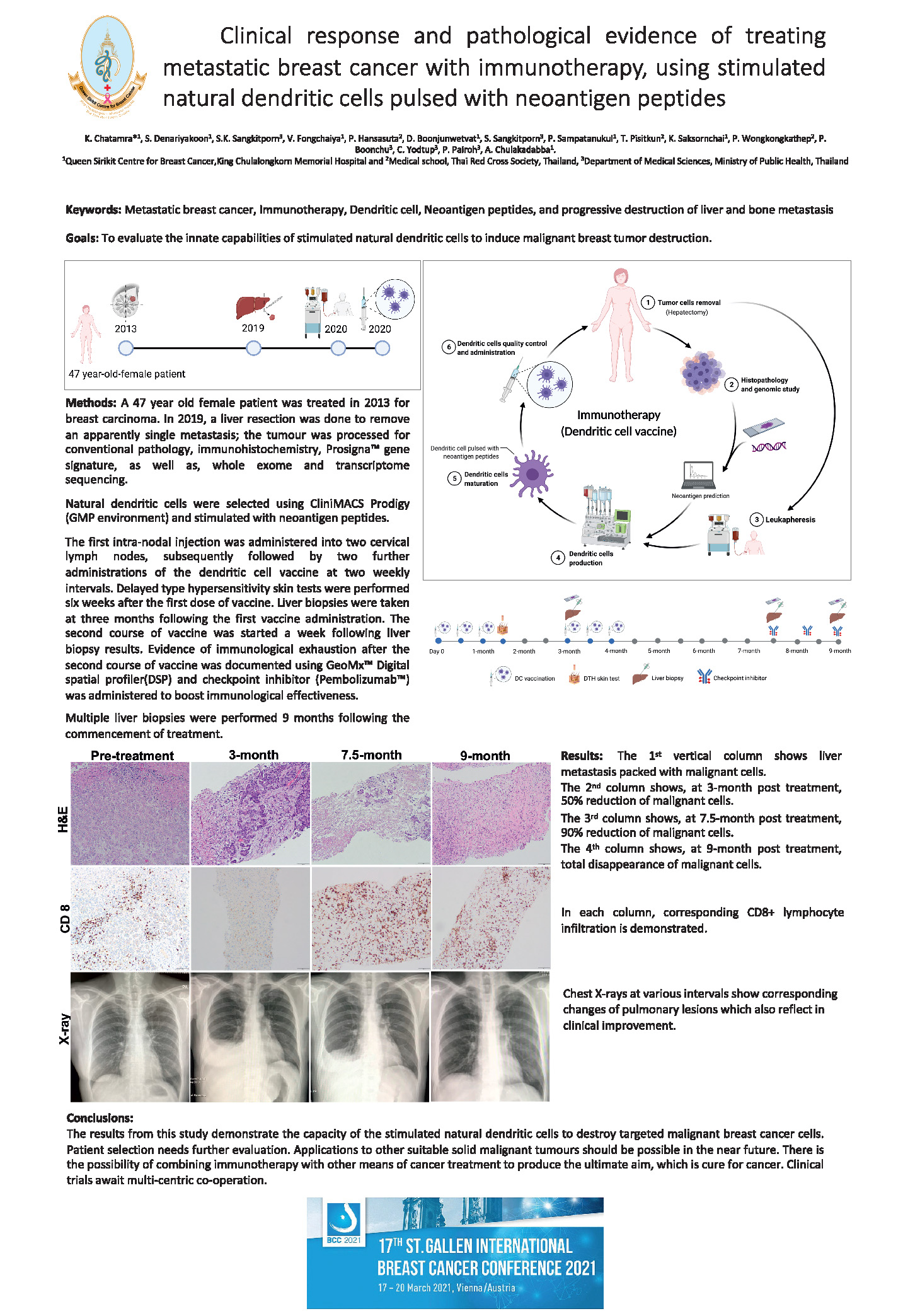
QSCBC’s new method using immunotherapy, by reintroducing the breast cancer patient’s own natural dendritic cells back into the patient’s cervical lymph nodes. These cells are then able to instruct the immune cells to recognise and destroy the breast cancer cells. The QSCBC has the CliniMacs Prodigy equipment and a class 100 international standard clean room (GMP standard), to produce the vaccine being given to the patient in the operating theatre, for maximum patient safety.
Immunotherapy Project


AN EXCITING NEW HOPE FOR BREAST CANCER PATIENTS
The QSCBC’s new approach to immunotherapy for metastatic breast cancer was presented at the St Gallen International Breast Cancer Conference in March 2021.

Phloenphit Kowid was the first patient to receive the new QSCBC immunotherapy method, which resulted in a complete reversal of her terminal metastatic breast cancer. Her successful treatment results were documented with full medical evidence, conclusively showing that her cancer had disappeared from her lungs and liver. She had been suffering from metastatic terminal breast cancer, (breast cancer which had spread to other organs), but despite following a conventional regimen of treatment, it ultimately failed, before immunotherapy was considered on compassionate grounds. There are no negative side effects associated with the QSCBC’s new immunotherapy method and the patient now has an excellent quality of life.
Immunotherapy uses the body’s own ability to fight invading organisms like bacteria and viruses, to prevent the body being infected. The immune system is the body’s own defence system against infection and any aberrant cells that develop in the body.
Immunotherapy is widely used to treat many types of conditions which involve the body’s immune system. This new approach to immunotherapy developed by the QSCBC, treats the spread of breast cancer into other organs, (the liver, lungs, bone), but it should not be confused with primary cancer in the liver, bone or lungs, as these cancer types have a very different make-up and need very different treatment methods. The breast tumour may have been treated successfully, but this new method aims to treat the spread of the breast cancer in the other organs. In the future it is hoped that other cancers can be treated with this new immunotherapy method devised by the QSCBC, namely, ovarian, prostate and bladder. Further evidence from the QSCBC’s clinical study will hopefully allow the new method of treatment to be applied to early breast cancer cases, so that ultimately, the disease can be potentially cured.
Immunotherapy can be used at a very superficial level, as seen in many commercial clinics worldwide. In contrast the QSCBC performs a highly complicated and in-depth involvement of the body’s cells in the immune system, which entails a very complex preparation and execution. The QSCBC team extracts very fragile natural dendritic cells and the ensuing culture and pulsing of these cells, carried out at the QSCBC, is a very delicate and difficult procedure. This approach can only be practised in specialist units with a multidisciplinary support and should be completely differentiated, and not confused with the aforementioned superficial methods. To date, immunotherapy with metastatic breast cancer patients had proved too difficult and dangerous. It should be emphasised that the QSCBC’s new method does not have any unpleasant or dangerous side effects for patients. The QSCBC’s new approach to immunotherapy has shown that two consecutive patients with metastatic (terminal) breast cancer, who have been treated with natural dendritic cells, pulsed with neoantigens (*specific peptides), had a complete pathological response, which indicates a complete destruction of all the breast cancer cells, demonstrated in both cases. This total eradication of breast cancer cells is backed with full medical and scientific evidence. The initial results have been so encouraging, a formal clinical trial is underway.
*Peptides are small proteins on the surface of all cells, they have many functions, including the ability to communicate, stimulate cell functions and recognise other cells.
The QSCBC also collaborates internationally on research trials, including intraoperative radiotherapy, having carried out well over 300 cases in the operating theatre; patients therefore only require one session rather than many spread over several weeks. The QSCBC has been linked with the UK for this trial for over ten years.
Another QSCBC clinical research trial that has directly impacted patients is a new treatment method devised for extensive locally advanced breast cancer. The QSCBC has produced a complex protocol for this specific work, which destroys the tumour and helps to close the chest wall and keep the omentum, part of the abdomen, viable in its new position, sealing the very large chest wound. The results have been very beneficial and wounds have been effectively sealed. A final skin graft over the omentum is done, so that cosmetically, it looks like the rest of the chest wall. The procedure offers real hope for patients with these huge lesions, rather than being left with a fungating tumour.
A scalp cooling equipment project has been adapted by the QSCBC team to alleviate a patient’s hair loss during chemotherapy treatment. It is based on the principle that by lowering the temperature of any organ the blood flow will be reduced. The amount of chemotherapy chemicals, carried by the blood to the hair follicles will automatically be greatly reduced, resulting in far less hair loss. The surviving hair follicles produce a healthy new crop of hair.
The cryoablation project is aimed at patients who have been identified as having a small malignant tumour. The cryoablation deeply freezes the malignant cells quickly causing the cells to burst and be destroyed. This method requires a minimal surgical procedure and should leave patients with the best cosmetic results. Cryoablation in the past has been used for benign lumps, which had the built-in disadvantage of leaving the patient with even larger lumps. The type of fibrous tissue making up a benign lump will swell and die, but will not disappear immediately; it may take from weeks to years before the lump is reabsorbed by the body.